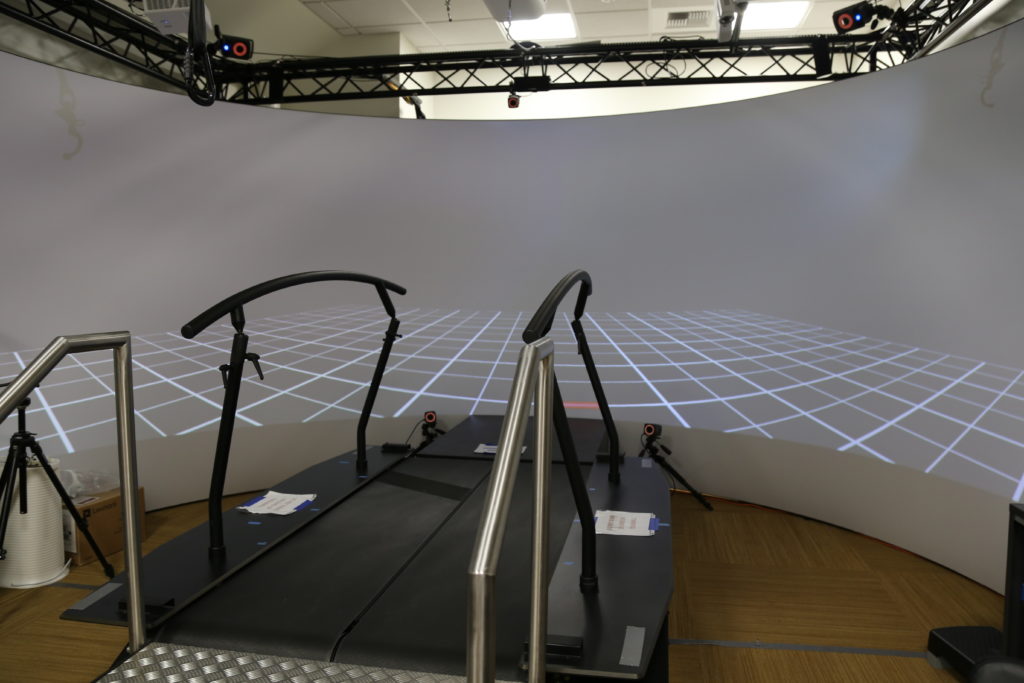
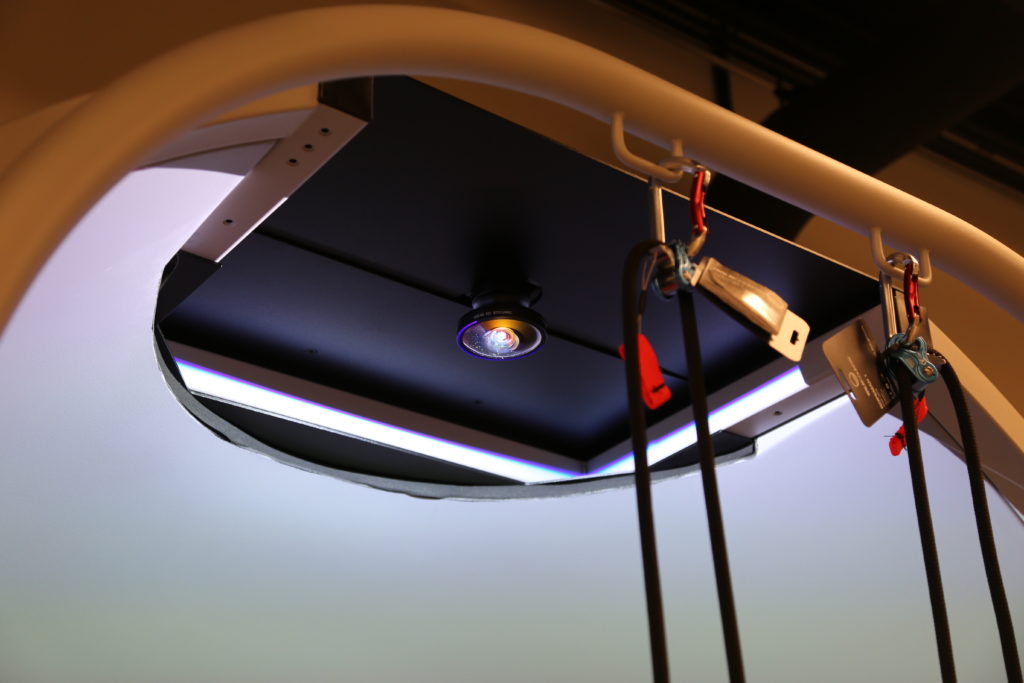
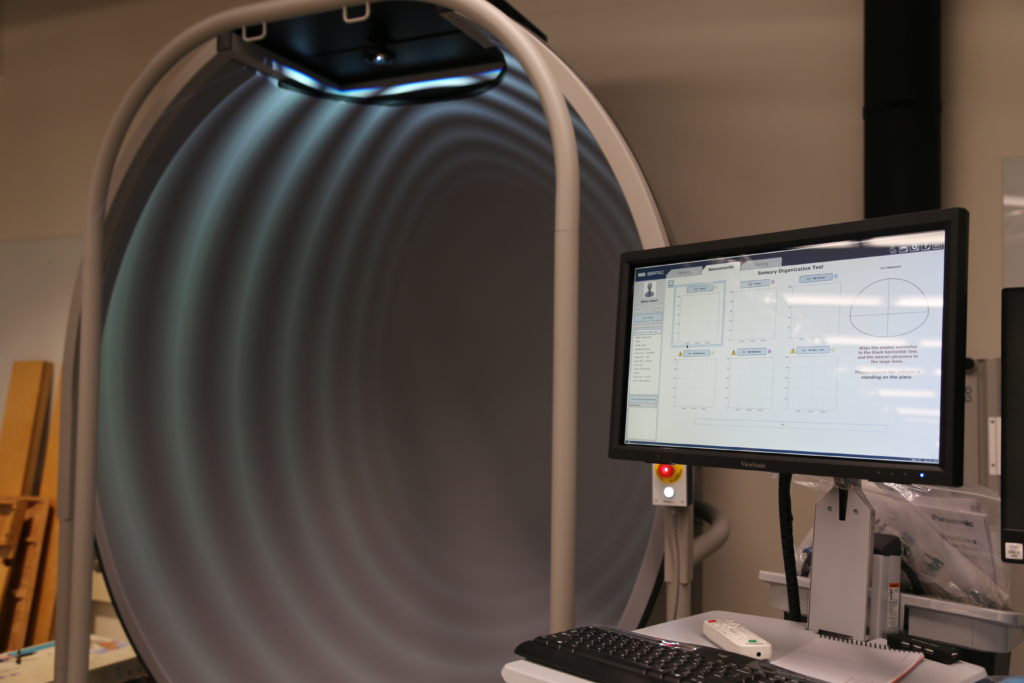
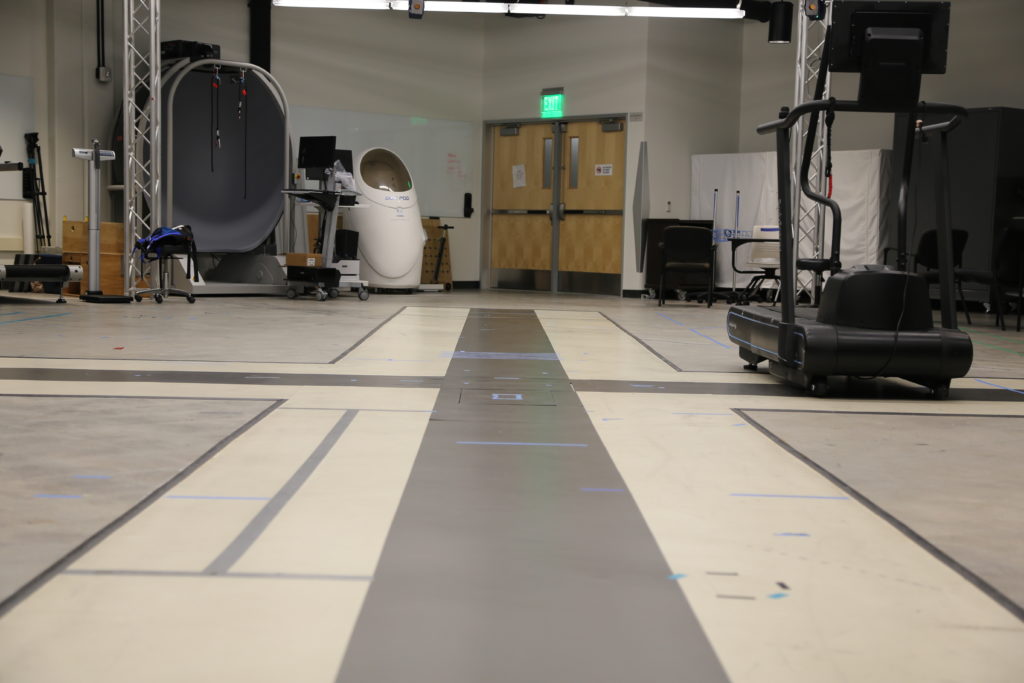
GAIT REHABILITATION & RESEARCH LAB
Revolutionizing Stroke Care: The Future of Fall Risk Assessment Using Smartphones
Stroke
Stroke is regarded as a ‘family disease’ since the lives of stroke survivors and their families change drastically, making it difficult to return to a pre-stroke lifestyle. The detrimental effects of falls include serious injuries, increased morbidity and mortality, dwindling functional mobility and quality of life, and high health-related costs. Most fall risk assessments for ambulatory post-stroke survivors are based on an ordinal scale of functional measurements, lack objectivity and accuracy, and are limited to clinical or laboratory environments. Early identification of post-stroke survivors at risk of falling is crucial for developing timely tailored interventions to reduce falls. Stroke survivors face a daunting challenge — the risk of falls. In the United States alone, the fallout from these incidents is not just a health concern but a significant socio-economic burden. Traditional fall risk assessments, usually conducted in clinical settings, have limitations in sensitivity and practicality. Recognizing these gaps, our team is pioneering a breakthrough approach to mitigate this risk, harnessing the power of technology and data science.
Fall Risk in Post-Stroke Patients












The App
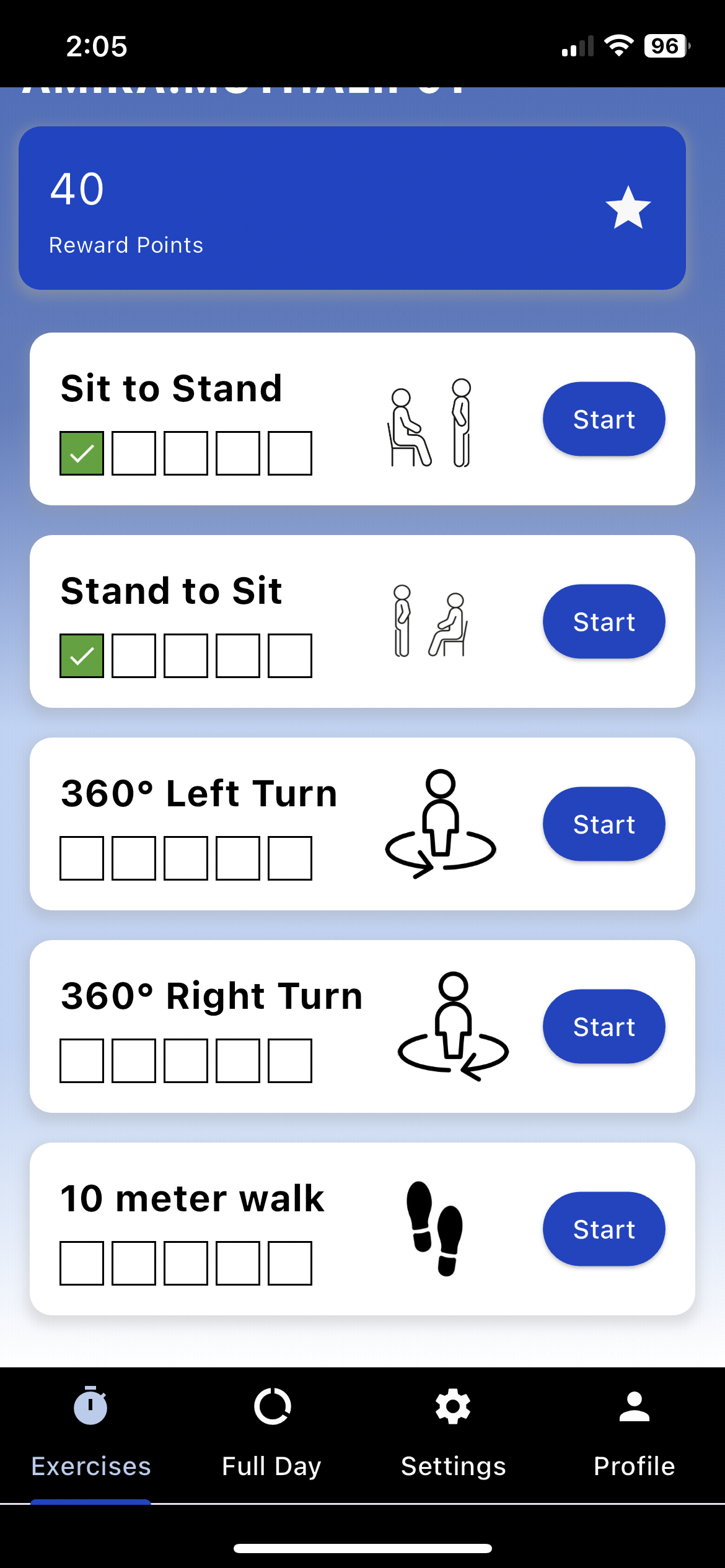
Functions
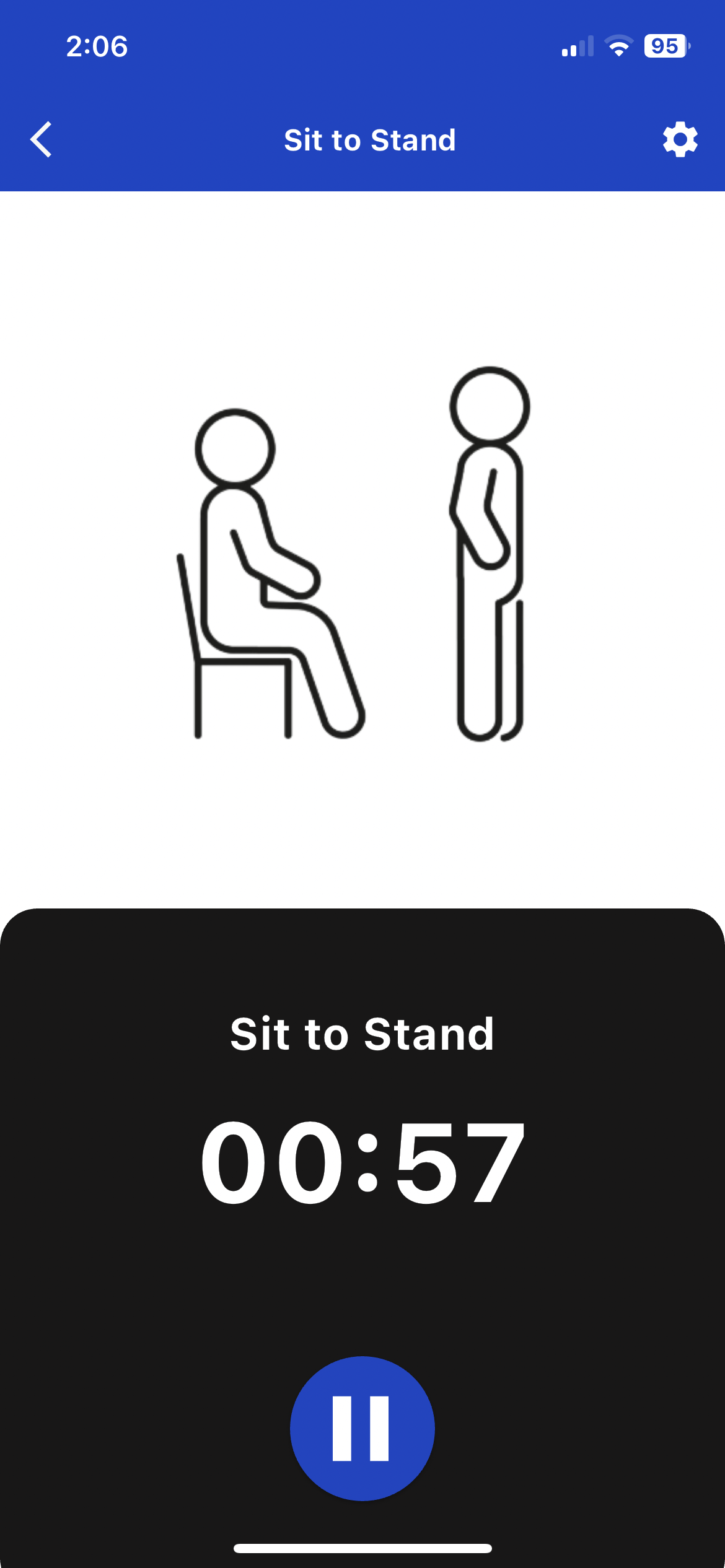
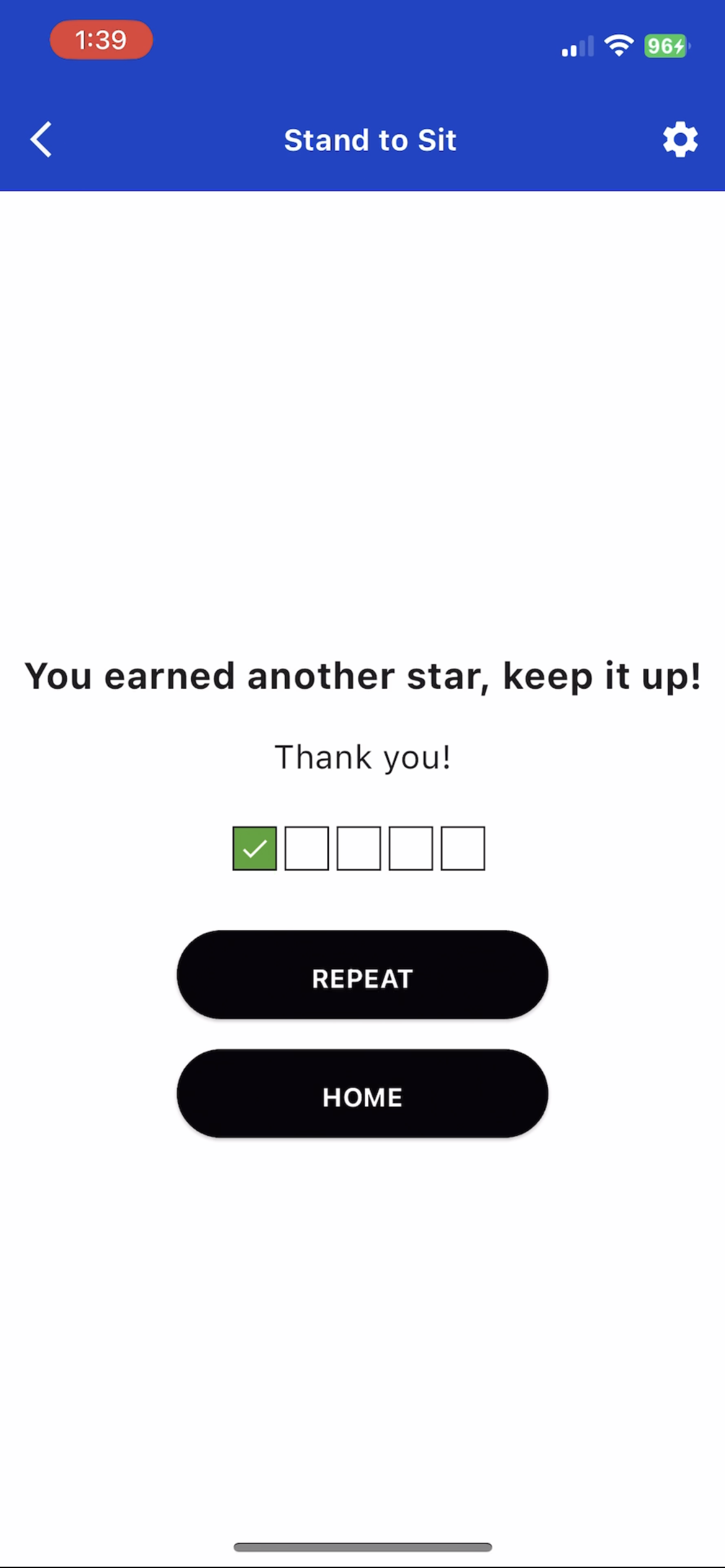
The app’s core functionality lies in its ability to process data from simple activities like walking, turning, and standing up. These daily actions, often overlooked, are critical in understanding the risk of falls post-stroke. By continuously and passively collecting data, the app provides a comprehensive view of the survivor’s mobility and balance, factors crucial in fall risk assessment.
Algorithm
The app employs advanced machine learning algorithms to analyze data collected from the smartphone’s inertial measurement unit (IMU). By monitoring activities like walking, sit-to-stand movements, and turning, the app identifies patterns and anomalies indicative of increased fall risk. By leveraging the ubiquitous nature of smartphones and their built-in sensors, the app provides a non-intrusive, continuous evaluation of fall risk.
What sets this project apart!
Traditional methods of fall risk assessment, often confined to clinical settings, face limitations in terms of practicality and accuracy. Our approach, however, captures the nuances of everyday movements in natural settings, offering a more accurate and personalized assessment.
Healthcare Industry
It promises to ease the burden on caregivers, reduce healthcare costs, and most importantly, improve the quality of life for millions of stroke survivors. This project is not just a technological innovation; it's a beacon of hope, signaling a new era in stroke rehabilitation and care. Our goal is clear: to create a world where stroke survivors can live with confidence, less fear of falling, and greater independence. This research is a testament to the power of technology in transforming healthcare. It's a step towards a future where data-driven solutions can significantly improve the lives of those living with the aftermath of a stroke.
Our Project's Aim
To establish if digital biomarkers extracted from the smartphone data while performing prescribed ADLs significantly differ between high and low-risk fallers in laboratory settings. The remaining data needed to build the ML model is collected entirely in the participant’s home setting. The participants will wear the smartphone on their waist during all waking hours and perform regular activities of daily living.
To train three ML models that can classify fall risk using different data modalities: i) passively collected 3-day ADL data ii) data from prescribed simple ADL tasks like turning, walking, and sit-to-stand iii) combined subjective and objective data.
To assess the predictive validity of the ML models against actual fall occurrences after six months.
Team
